Secondary Trauma in Mental Health Professionals
Secondary Trauma in Mental Health Professionals
The mental health field continues to grow, with over one million professionals working as of 2021. In the wake of the pandemic, demand for therapeutic resources has surged, leading to higher caseloads and increased emotional demands. This rising pressure can blur the lines between a client’s experiences and a therapist’s well-being. Recognizing and addressing signs of burnout and secondary trauma is essential to maintaining professional and personal resilience.
Bring HopeNation Campus to your Students
Understanding Secondary Trauma
Secondary trauma refers to the emotional and behavioral impact of a mental health professional’s work on their own well-being. Mental health workers are trained to offer empathy and provide a safe space for clients to process emotions. While rewarding, this work can be emotionally taxing. The deep empathy required for the job often leads therapists to absorb their clients' emotions, especially with high caseloads and extended working hours.
Types of Secondary Trauma
1. Compassion Fatigue (CF)
Compassion fatigue is the emotional and physical exhaustion that arises from working with specific populations. Research highlights that a professional’s personal trauma history and heightened empathy levels are predictors of compassion fatigue. Professionals who deeply connect with their clients’ struggles may experience CF more acutely, as the emotional resonance makes the challenges feel personal.
2. Vicarious Trauma (VT)
Vicarious trauma occurs when mental health professionals develop symptoms of post-traumatic stress through their work with clients. Unlike compassion fatigue, VT doesn’t require the therapist to experience trauma firsthand. Instead, detailed exposure to clients’ traumatic experiences can lead to feelings of distress, hyperarousal, and avoidance in the professional.
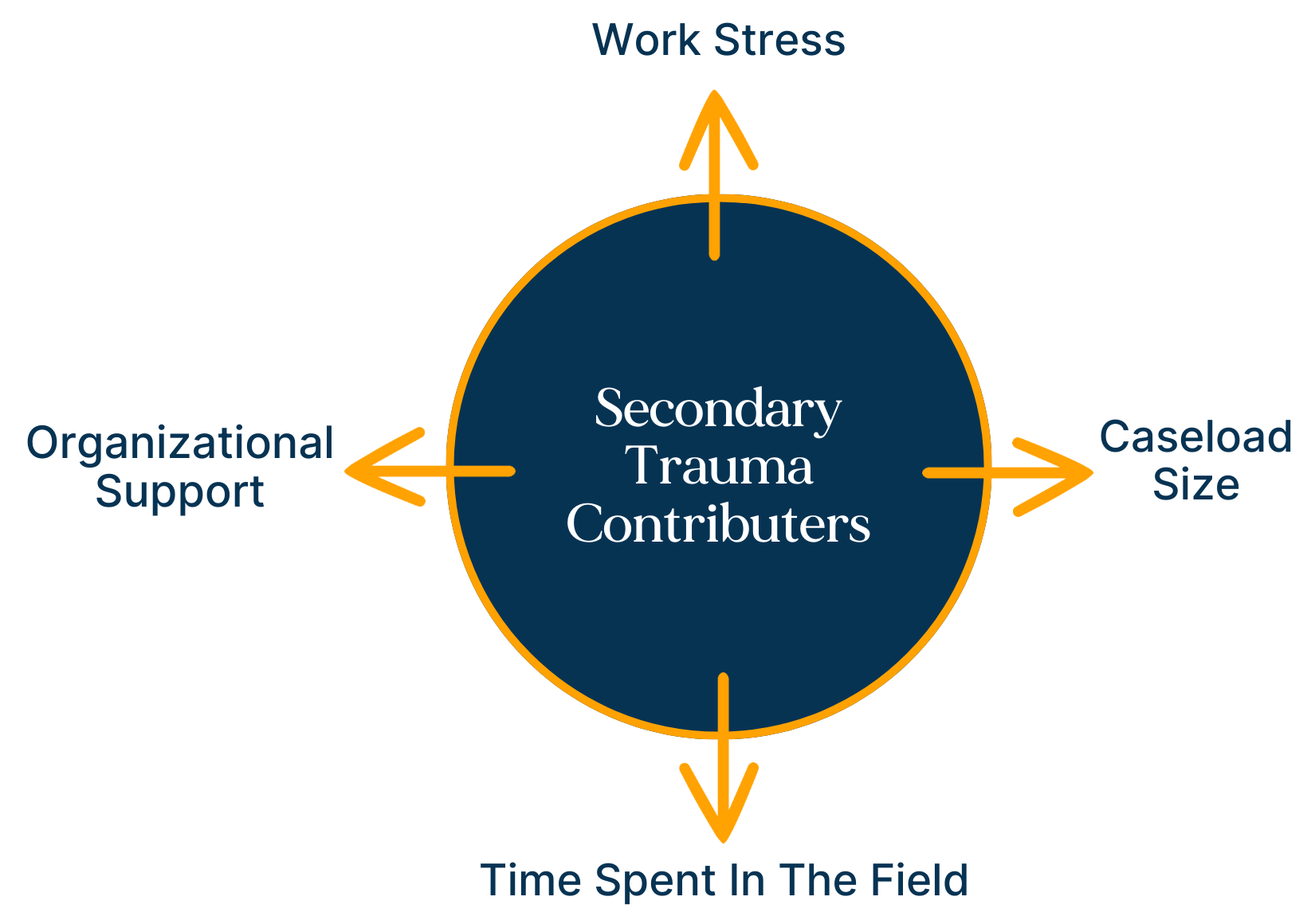
What Contributes to Secondary Trauma?
A study of 152 professionals in Australia identified key factors contributing to secondary trauma, including:
Work stress and caseload size
Time spent in the field
Organizational support
Interestingly, working with trauma clients was found to be a less significant predictor of secondary traumatic stress than the length of time spent in the field and higher levels of empathy. This suggests that while trauma cases are challenging, a professional’s longevity in the field and emotional investment play a larger role in secondary trauma.
How Organizations Can Support Mental Health Professionals
Organizations can play a vital role in reducing secondary trauma by fostering a culture of openness and support.
Use Assessment Tools:
Implement tools like the Secondary Traumatic Stress Scale (DSM) or the Compassion Fatigue Assessment to measure employee well-being. Anonymous results can help organizations identify stress patterns and address gaps in support.Encourage Open Communication:
Create a safe environment for employees to share feelings of burnout and stress without fear of judgment or retribution.Host Workshops and Follow-Ups:
Provide team-building exercises and self-care workshops, with follow-ups to ensure employees apply what they’ve learned.
When employees feel heard and valued, they’re more likely to prioritize their well-being and perform at their best.
Strategies to Combat Secondary Trauma
For New Professionals:
Seek mentorship from seasoned therapists to learn how to recognize and manage signs of secondary trauma.
For Experienced Professionals:
Set Time Boundaries: Define start and stop times for tasks like note-taking and administrative work, and schedule adequate breaks.
Seek Peer Support: Share challenging cases with trusted colleagues for guidance and perspective.
Prioritize Personal Time: Dedicate time each day to unwind through hobbies or activities you enjoy.
Lean on Your Support System: Confide in trusted friends or family members about your struggles, even if you can’t share specifics due to confidentiality.
Practice Self-Work: Journaling, creating art, and engaging in mindfulness practices can help release emotional tension. Physical activity, whether solo or in a group, is also beneficial for relieving stress.
Final Thoughts
Trauma is an inevitable part of the mental health profession, and the longer one works in the field, the more exposure they have to its challenges. However, by actively prioritizing self-care and fostering supportive organizational cultures, professionals can build resilience and sustain their passion for helping others. Protecting your well-being isn’t just a professional necessity—it’s a personal one, ensuring both career longevity and overall life satisfaction.
✓ Medically Reviewed By Casey Merrill, LPC-MHSP